Chennai's Silent Poison Crisis: Rat Killers Claim Hundreds of Victims
Last week, a gig worker in Chennai made headlines by refusing to deliver rat poison to a woman. He suspected she might use it to harm herself. This incident spread quickly across social media platforms. Meanwhile, inside government hospital wards across the city, doctors were having a more urgent conversation. They discussed a grim reality: rodenticides poison hundreds of people in Chennai every single year.
These poisons attack vital organs like the liver and heart with devastating speed. Often, medical intervention comes too late to prevent severe damage or death.
Official Records Paint a Stark Picture
Toxicology department data from Chennai's government hospitals presents a clear hierarchy of danger. Rat poison consistently leads the list of poisoning cases. It is followed by snake bites and a highly toxic liquid herbicide known as paraquat.
Doctors explain that rat poison is sold in various forms, including paste, powder, and cakes. When consumed in significant amounts without treatment, it causes severe cellular poisoning. The damage progresses systematically, affecting the liver, heart, and brain, ultimately leading to fatality.
How These Common Poisons Work Inside the Body
Dr. S. Chandrasekar, head of the medicine department at Government Stanley Medical College Hospital, provided a detailed breakdown. "The commercially available cakes typically contain warfarin or superwarfarin," he said. These substances block vitamin K in the body, which is crucial for blood clotting. The result is uncontrolled internal bleeding.
Pastes and powders often contain a different, equally dangerous compound: zinc phosphide. "This chemical reacts with stomach acid," Dr. Chandrasekar added. "It releases phosphine gas, which is deadly. It starves cells of energy, leading directly to liver failure. Many patients who ingest these require liver transplants."
A Critical Treatment Window and Alarming Statistics
One of the most dangerous aspects of this poisoning is its delayed onset. Patients frequently show no visible symptoms for up to 24 hours after consumption. "If they report to us within this window, we can act," Dr. Chandrasekar stated. Treatment involves a stomach wash, administration of vitamin K, and N-acetyl cysteine. This combination helps restore blood clotting functions and prevents further liver damage.
For severe cases, doctors recommend a plasma exchange procedure. This involves removing the poisoned plasma from the patient's blood and replacing it with fresh plasma or fluids.
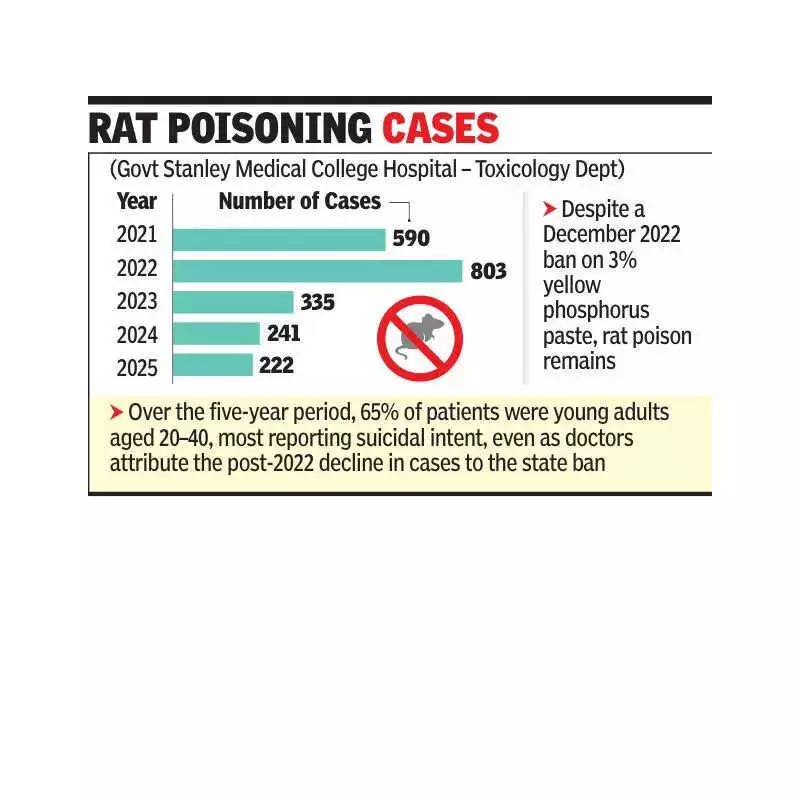
The statistics from Government Stanley Medical College Hospital are alarming. In 2025 alone, the hospital recorded 222 cases of rat poison ingestion. A significant 65% of these patients were aged between 20 and 40, with a majority being men. Another 24% were under the age of 20.
Looking at a broader timeline from 2021 to 2025, the hospital documented a total of 2,191 cases. The peak occurred in 2022 with 803 cases. Dr. Chandrasekar noted a regulatory intervention. "At the end of 2022, Tamil Nadu banned the sale and use of 3% yellow phosphorus paste," he said. This was the most commonly used poison for self-harm. "Since that ban, we have seen a decline. The 222 cases in 2025 reflect this decrease."
Geographic Origins and Available Support
Most cases do not originate in Chennai city itself. They predominantly come from northern agricultural districts like Cuddalore, Villupuram, and Kallakurichi. Chennai accounts for only a small fraction of the total incidents.
Doctors observe that in most adult cases, the consumption of rat poison is intentional. However, accidental ingestion remains a common and tragic occurrence among young children.
For individuals experiencing distress, support is available. The Tele MANAS national mental health helpline can be reached at 14416. The statewide health helpline is 104. These services offer crucial support and guidance.