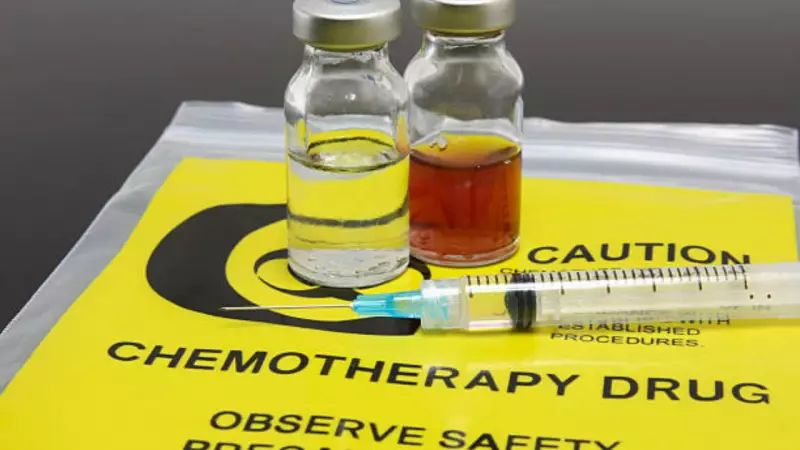
For decades, the word 'cancer' has been almost synonymous with 'chemotherapy' in the public mind. The powerful image of hair loss, nausea, and hospital visits has cemented chemo as the default treatment. However, medical science is moving beyond this one-size-fits-all approach, especially for early-stage breast cancer patients.
Breaking the Chemotherapy Myth in Cancer Care
Dr. Rohan Khandelwal, Head of the Breast Centre at CK Birla Hospital in Gurugram, highlights a common fear. The moment a patient is diagnosed with breast cancer, one of their first questions is whether they will need chemotherapy. The dread stems from widespread awareness of its significant side effects and the potential impact on quality of life. Many believe chemo is unavoidable, regardless of the cancer's stage.
"The good news is that with advances in medicine, doctors are now rethinking chemotherapy for early-stage breast cancer patients," says Dr. Khandelwal. The decision is no longer automatic but is driven by a detailed understanding of the individual's disease.
How Doctors Decide: Biology Over Assumption
The key, according to Dr. Khandelwal, is a thorough assessment of the cancer's stage and biology. Treatment plans are now highly personalised.
For aggressive tumours at a later stage, chemotherapy often comes first, followed by surgery. Conversely, for patients with early-stage disease and favourable tumour biology, chemotherapy might be safely avoided. Another group undergoes surgery first if the tumour is operable and less aggressive. The decision for further therapy like chemo or radiotherapy is then based on post-surgery results.
"Our focus is always on disease-free survival and overall survival," explains Dr. Khandelwal. "If the patient is going to substantially benefit from chemotherapy, then they are a candidate for it. If they don't have an absolute benefit, there is no strong reason for giving them the side effects of chemo."
The Power of Personalisation: A Case for De-escalation
Dr. Khandelwal cites the example of a 52-year-old early-stage patient who experienced a sudden spike in hypertension and a minor stroke during recovery. She qualified for a molecular test, which indicated a low-risk tumour, allowing her to safely avoid chemotherapy.
"The treatment is more biology-driven," he states. For a specific subset of patients—those with early-stage, hormone-positive breast cancer—molecular tests can assess recurrence risk. A low-risk result can mean avoiding chemotherapy and its associated trauma.
This 'de-escalation' of treatment, backed by scientific evidence, directly improves a patient's quality of life. Chemotherapy's side effects, like hair loss, are not just physical but deeply emotional. While often reversible, the experience can be traumatic, and some effects may be long-lasting.
"Any patient would be happy when you tell them they do not need chemo. Chemotherapy is the most dreaded part of cancer," Dr. Khandelwal concludes. The modern oncologist's goal is to personalise care, ensuring patients only undergo tough treatments when the benefits unequivocally outweigh the burdens.