The alarming case of a 14-year-old boy from Surat, who recently underwent a life-saving liver transplant in Mumbai, has thrown a harsh spotlight on the growing crisis of fatty liver disease among Indian adolescents. Once considered an adult ailment, severe fatty liver is now striking teenagers, with doctors pointing to a dangerous cocktail of genetic predisposition, rampant junk food consumption, and rising obesity.
A Life Saved by a Father's Donation
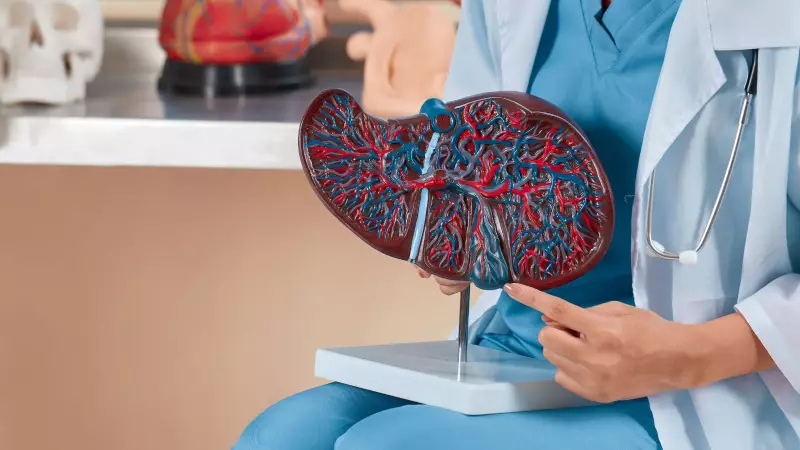
The teenager was admitted to Sir H. N. Reliance Foundation Hospital in Mumbai with acute liver failure, a direct consequence of an advanced form of fatty liver disease. His condition was critical, marked by severe jaundice, massive fluid accumulation in the abdomen (ascites), and extreme water retention that caused a sudden weight gain of 15-20 kg. With his own liver unable to perform vital functions like filtering toxins, a transplant became the only viable option.
In a poignant turn, the boy's father stepped forward as the living donor, giving a portion of his right liver lobe to save his son. The surgery, conducted just a month ago, was successful. The boy is now recovering at home, with his bilirubin levels normalized and all symptoms of liver failure resolved. His weight, which had ballooned to 84 kg due to fluid overload, has now stabilized in the low 60s.
The Hidden Genetic Trigger Accelerated by Diet
Investigations into the rapid deterioration revealed a crucial factor: multiple genetic mutations. The boy carried high-risk variants in genes like PNPLA3 and GCKR, which are known to significantly increase susceptibility to fat accumulation in the liver and are notably prevalent in the Indian population.
However, genetics alone did not seal his fate. Doctors emphasize that lifestyle acted as a powerful accelerator. "A person with high genetic risk may never develop severe disease if they maintain a healthy lifestyle," explained Dr. Gaurav Gupta, Co-director of the Department of Liver Transplant and HPB Surgery. "But like many teens, this boy regularly consumed ultra-processed and junk foods, which accelerated the damage."
Dr. Arti Pawaria, Chief Paediatric Hepatologist, confirmed that his diet was packed with hazardous items typical of teen preferences: packaged snacks, chips, burgers, cookies, noodles, and sugar-laden sodas. This pattern of excess calories and low physical activity overwhelmed his liver, turning a genetic predisposition into a life-threatening reality.
A Wake-Up Call for Families and Policymakers
This case is a stark indicator of a broader trend. Fatty liver disease is now the most frequent cause of chronic liver disease in adolescents, affecting an estimated 10-17 percent of teenagers with obesity. The incident underscores an urgent need for collective action.
Medical experts are calling for a multi-pronged approach to prevent such crises:
- Family-Driven Lifestyle Changes: Prevention must start at home. Families should aim for five daily servings of vegetables and fruits, choose whole grains and lean proteins, and replace sugary drinks with water or infused water.
- Early Dietary Discipline: Encouraging fresh, home-cooked meals with plenty of vegetables, fruits, pulses, and milk-based proteins is crucial. Reading labels to avoid hidden sugars is essential.
- Holistic Habits: Experts recommend eating together without screens, involving teens in cooking, ensuring 9-10 hours of sleep, limiting screen time, and exercising as a family.
For the young transplant recipient, the journey continues. He will be on immunosuppressant medication for life and must adhere strictly to a healthy lifestyle to protect his new liver. However, his prognosis is good; with careful management, he can resume school, play sports, and lead a normal adult life.
The message from hepatologists is clear: Childhood obesity and poor dietary choices are no longer just about weight—they are silent sculptors of liver health, with potentially devastating consequences. Early intervention at the family and community level is the most powerful medicine to avert a looming epidemic of advanced liver disease in India's youth.





