The Karnataka Health and Family Welfare Department has initiated a significant restructuring of its mother and child health (MCH) services. The move, termed 'rationalisation,' involves a large-scale redeployment of specialists, which will lead to the downgrading of numerous Community Health Centres (CHCs) across the state. The primary goal is to tackle the state's persistently high maternal mortality ratio by ensuring critical care is available where it's needed most.
Addressing the Core Issue: Preventing Maternal Deaths
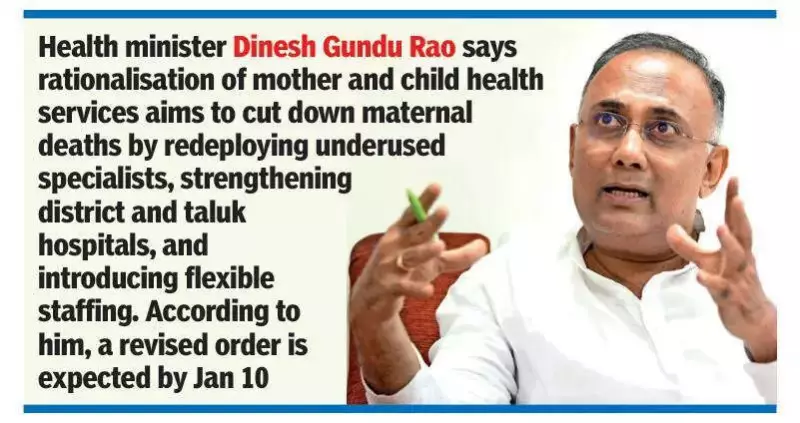
In an exclusive interview, Health Minister Dinesh Gundu Rao outlined the driving force behind this major policy shift. He pointed to Karnataka's higher maternal mortality ratio compared to neighbouring states like Tamil Nadu, Kerala, and Telangana. The key problem identified is the delay in accessing emergency services. "An emergency happens, the woman goes to a taluk hospital, there is no facility, she is shifted again, becomes critical on the way, and by the time she reaches the district hospital, it is too late," Rao explained, describing the tragic chain of events the government aims to break.
The minister acknowledged concerns about potential service gaps, especially given existing staff vacancies. He admitted the change is substantial and has faced resistance but believes it will strengthen the healthcare system in the long term. The department is already working on modifications to the original order issued on November 7 to include certain necessary CHCs.
Optimising Resources and Introducing Flexibility
The rationalisation is fundamentally about better utilising existing medical personnel. Rao highlighted the current imbalance: many CHCs have gynaecologists with minimal workloads, some handling zero to ten deliveries a month, while district hospitals are overwhelmed. Simultaneously, taluk hospitals often lack doctors after hours, becoming hotspots for maternal emergencies.
Distance mapping is a critical criterion for the reshuffle. CHCs in remote or hard-to-reach areas will remain untouched, regardless of performance metrics, to prevent forcing communities to travel farther. The plan also involves redeploying MBBS doctors from posts with little clinical work.
A crucial reform is the revision of the specialist 'triad' model required for a fully functional CHC. Traditionally, this consisted of a gynaecologist, an anaesthetist, and a paediatrician. The government is now introducing flexibility. "Instead of only a paediatrician, a physician can also be part of the triad. In many places, a physician is actually more useful because they can handle a wide range of medical cases," stated Rao. This change acknowledges the practical challenges of staffing and aims to make the model more adaptable to local needs.
Revised Order and New Recruitment on the Horizon
The health minister provided a clear timeline for the next steps. A modified government order incorporating the adjustments is expected to be notified by January 10. This will be followed by a major recruitment drive for 230 doctors, including both specialists and MBBS graduates, to fill the system's gaps.
Furthermore, the return of around 100 doctors who had gone for postgraduate studies, including approximately 40 specialists, will provide an immediate boost to the state's medical workforce. Their deployment will be aligned with the new rationalisation plan. The overarching objective remains steadfast: to create a more efficient, responsive, and life-saving network for mothers and children across Karnataka.