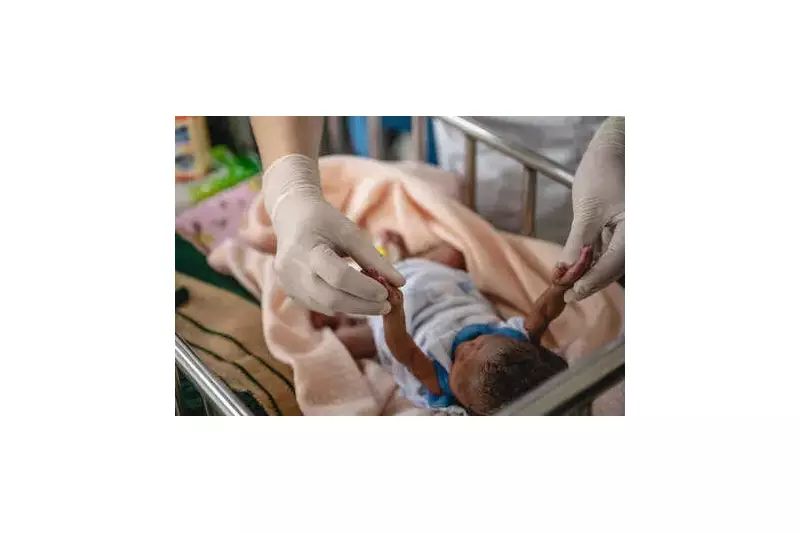
Post-Pandemic Stillbirth Crisis: India Records 44% Increase in Late-Term Fetal Deaths
A comprehensive national study has uncovered a disturbing trend in India's maternal healthcare landscape. Even as hospital deliveries resumed following the Covid-19 pandemic, the country witnessed a sharp escalation in babies dying just before birth during the post-pandemic period. This alarming finding emerges from a major research initiative analyzing births across India between 2019 and 2022.
Study Methodology and Scope
The research, published in the esteemed journal BMC Pregnancy and Childbirth, was conducted by experts from the Public Health Foundation of India with crucial support from the Indian Council of Medical Research. This landmark investigation represents one of the most extensive examinations of stillbirth patterns in recent Indian history, drawing from a nationally representative mortality survey encompassing nearly one million individuals across nine diverse states.
The study spanned Assam, Gujarat, Haryana, Jharkhand, Kerala, Maharashtra, Odisha, Tamil Nadu, and Uttar Pradesh, providing a comprehensive geographical representation of India's varied healthcare landscapes.
Quantifying the Crisis: Statistical Evidence
The data reveals a troubling progression in India's stillbirth rates across different phases of the pandemic. Before Covid-19, the rate stood at 12.7 per 1,000 births. During the pandemic period, this increased to 14.4 per 1,000 births. However, the most dramatic surge occurred in the post-Covid period, with rates climbing sharply to 18.3 per 1,000 births.
This represents a staggering 44% increase between the pre-Covid and post-Covid periods, highlighting how healthcare disruptions during the pandemic have created lasting consequences for maternal and fetal health.
Geographical and Healthcare Disparities
The increase proved most pronounced in rural regions, where rates reached nearly 20 per 1,000 births, compared to approximately 14 in urban areas. This disparity underscores significant gaps in access to timely antenatal care and emergency obstetric services in India's hinterlands.
The study's detailed analysis of 745 stillbirth cases revealed complex patterns in healthcare utilization. Public hospitals accounted for 44.7% of stillbirths, private hospitals for 39.2%, and home deliveries for 16.1%. However, these proportions varied dramatically across states, reflecting differences in health system utilization patterns rather than state-specific stillbirth rates.
Notable state-wise patterns included:
- Kerala (66.7%), Gujarat (60%), and Haryana (50%) reported majority stillbirths from private hospitals
- Odisha (72.6%), Assam (69.6%), Maharashtra (54.8%), and Tamil Nadu (54.6%) recorded most stillbirths in public hospitals
Clinical Insights and Systemic Failures
Perhaps most concerning is the timing of these tragedies. More than half of all stillbirths occurred at nine months of pregnancy or later, often just days before anticipated delivery. This pattern points directly to failures in late-pregnancy monitoring and delivery-time care rather than early pregnancy complications.
Dr. Renu Gupta, Director of Obstetrics & Robotic Gynaecology at Sri Balaji Action Medical Institute in Delhi, provides crucial clinical perspective: "The rise in late-term stillbirths indicates failures in timely risk detection and intervention, not gaps in early pregnancy care. Following Covid-19, third-trimester monitoring—including blood pressure checks, fetal growth assessments, movement tracking, and Doppler studies—has become inconsistent, particularly in overburdened public hospitals."
Dr. Gupta further explains: "Referral delays, staff shortages, and inadequate transport systems mean warning signs are frequently missed. While delivery numbers have recovered to pre-pandemic levels, the quality and continuity of care have not rebounded accordingly, leading to preventable losses just before birth."
Systemic Challenges and Documentation Gaps
The study identified multiple systemic challenges contributing to this crisis:
- Nearly one in five women whose babies were stillborn had been referred between facilities during labor, sometimes being sent back only to return later
- Only about one-third of mothers received explanations about why their baby died
- Despite mandatory registration requirements, merely 1% of stillbirths were officially documented, keeping most cases outside official records
Emotional Impact and Family Experiences
Beyond statistical measures, the research highlighted profound emotional consequences for affected families. Nearly half of mothers neither saw nor held their stillborn babies, often due to family decisions or medical advice. These findings underscore how stillbirths represent not just medical statistics but deeply personal tragedies that families often grieve in private.
Future Implications and Policy Concerns
Researchers issued a stark warning about India's ability to meet its public health targets. Without substantial improvements in antenatal surveillance, faster referral systems, and enhanced quality of care during labor and childbirth, India risks missing its goal of achieving a single-digit stillbirth rate by 2030 under the India Newborn Action Plan.
This study serves as a crucial wake-up call for healthcare policymakers, administrators, and practitioners across India. It emphasizes that restoring pre-pandemic service levels is insufficient—what's needed is a fundamental strengthening of maternal healthcare systems to prevent these late-term tragedies and ensure safer pregnancies for Indian women.





