Politics
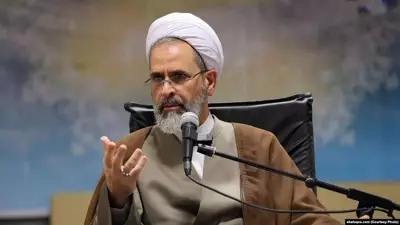
Iran Appoints Ayatollah Alireza Arafi as Interim Supreme Leader After Khamenei's Death
Iran has appointed Ayatollah Alireza Arafi as interim Supreme Leader following the death of Ayatollah Ali Khamenei in US-Israeli airstrikes. Arafi, a senior cleric, faces steering the nation amid regional tensions and internal uncertainty.
World
Ayatollah Alireza Arafi Appointed to Iran's Leadership Council After Khamenei's Death
Ayatollah Alireza Arafi has been appointed to Iran's Leadership Council, which will assume the role of the supreme leader following the killing of Ayatollah Ali Khamenei in a US-Israel joint operation.
Business
Stock Markets Brace for Volatile Week as Middle East Conflict Escalates
Indian stock markets are expected to open with a negative bias as escalating US-Israel-Iran conflict raises crude prices and geopolitical risks, with analysts warning of prolonged impact on equities.
Entertainment
BRIT Awards 2026 Chaos: Sombr Pushed Off Stage Mid-Performance in Shocking Incident
A shocking incident at the 2026 BRIT Awards saw rising star Sombr pushed off stage during his performance, sparking chaos and security concerns before a surprising twist emerged.
Sports
Lifestyle
Technology
White House AI Designation Threatens Google, Amazon, Microsoft Billions
Dean Ball warns the White House's 'supply chain risk' tag on Anthropic could force Google, Amazon, and Microsoft to divest billions, calling it 'attempted corporate murder' and chilling US AI investment.
Grok AI's 'Prediction' of Iran Strike Debunked as Coincidence
A viral claim that Elon Musk's AI chatbot Grok predicted the date of US-Israel military action against Iran is false, stemming from a hypothetical exercise, not real foresight.
US DPA Threat Against Anthropic AI Ends in Defense Ban
The Pentagon's ultimatum to Anthropic using the Defense Production Act has concluded with the AI company being barred from defense applications. This marks a significant shift in how the decades-old law could be applied to technology firms.
Fortnite Love and Legends Final Power Hour Event Details
Fortnite's Love and Legends Power Hour event concludes on March 1, 2026, offering exclusive Candy Hearts and cosmetics. Get timings for all regions and details on loot.
Honor Magic V6 Launched with Near-Creaseless Display
Honor has unveiled the Magic V6 foldable smartphone, featuring a nearly creaseless inner display and advanced hinge technology, ahead of its showcase at MWC 2026.
Health
Get Updates
Subscribe to our newsletter to receive the latest updates in your inbox!
We hate spammers and never send spam