A simple common cold could have been fatal for Cora Oakley. Born in Morristown, New Jersey, she entered the world with virtually no immune system, diagnosed with a rare and severe genetic condition known as Severe Combined Immunodeficiency (SCID). This illness, often called 'bubble boy disease', leaves the body defenceless without key white blood cells. For decades, a diagnosis meant a desperate race against time for a bone-marrow transplant. Today, thanks to a revolutionary gene therapy, Cora and 61 other children are not just surviving but thriving, their immune systems fully restored.
The SCID Challenge and a Mother's Fight
Cora's mother, Chelsea Ferrier, described the heartbreaking paradox of SCID. "It seems like you have this perfectly healthy child who's happy and hitting her milestones," she said. "But no - she is sick. She can't do anything. She can't go outside." The standard cure was a bone-marrow transplant, most effective with a perfectly matched sibling donor. Cora, however, was Ferrier's first and long-awaited "miracle" child after three years of trying and several miscarriages.
In the United States, up to 100 infants are born with SCID each year, caused by defects in more than 20 different genes. Cora had a specific type called ADA-SCID. In 2017, a lifeline emerged: a clinical trial for a new gene therapy that could fix a patient's own stem cells, eliminating the need for a donor. "I would have sold my organs to get into that trial," Ferrier stated. Cora secured the final spot.
How the Gene Therapy Breakthrough Works
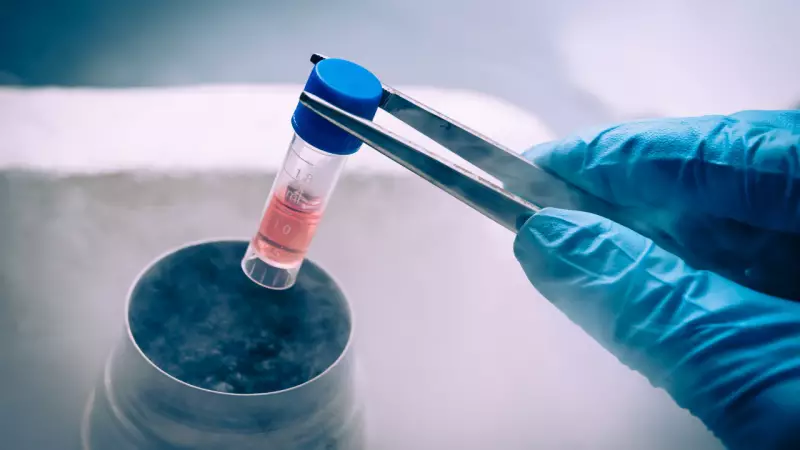
The science behind this treatment is as ingenious as it is life-saving. Since SCID stems from a faulty gene, doctors collect the baby's own stem cells. In a laboratory, scientists use a harmless, disabled form of the Human Immunodeficiency Virus (HIV) as a courier to insert a healthy copy of the gene into these cells. This modified virus excels at delivering its genetic cargo into the cell's DNA without causing disease.
The corrected stem cells are then infused back into the child. Dr. Donald Kohn, a paediatric immunologist at UCLA Health who led the landmark study, explained the advantages. Babies need only a low dose of chemotherapy, and because the cells are their own, there is minimal risk of rejection and no need for long-term immunosuppression. The recovery is quicker with fewer long-term side effects compared to traditional bone-marrow transplants.
The results, published recently, are stunning. Researchers followed 62 babies with ADA-SCID who received this gene therapy. After nearly eight years, every single child was alive. In about 95% of them, including Cora, the therapy fully restored their immune systems. "This was a fairy tale 20 years ago," said Frank Staal, a stem cell researcher at Leiden University Medical Center. "Now it's a reality."
The Road Ahead: Accessibility, Cost, and Caution
Despite the success, challenges loom large. The treatment remains incredibly expensive, with costs running into millions of dollars per patient. Currently, no pharmaceutical company is ready to commercialise it. Dr. Susan Prockop, a paediatric specialist at Boston Children's Hospital, noted that the therapy exists only in trials funded by nonprofits and state agencies. "It's pretty rare that we have disorders that we can completely cure... but that doesn't mean much if families can't get it," she added.
Doctors also urge cautious optimism. While bone-marrow transplants have a decades-long track record, gene therapy's history is measured in years. Dr. Richard O'Reilly of Memorial Sloan Kettering Cancer Center pointed out that the long-term durability of the repaired immune system and potential risks are still being studied.
For families, even with treatment, SCID is a lonely journey filled with anxiety. "Parents of SCID patients are permanently anxious because they know one infection can take their child from them," Dr. Kohn said. Families must rigorously shield their babies from germs while the new immune system establishes itself.
Today, gene therapies are being tested for four of SCID's subtypes, which could collectively help two-thirds of all babies born with the disease. For Cora Oakley, life is now wonderfully ordinary. She is a fearless 8-year-old who loves animals and enjoys a childhood her mother once feared was impossible. "I don't ever want to think about what it would've meant," Ferrier said, "if Cora didn't have this opportunity." This story of medical triumph offers profound hope and highlights the urgent need to make such advanced treatments accessible globally, including in nations like India.