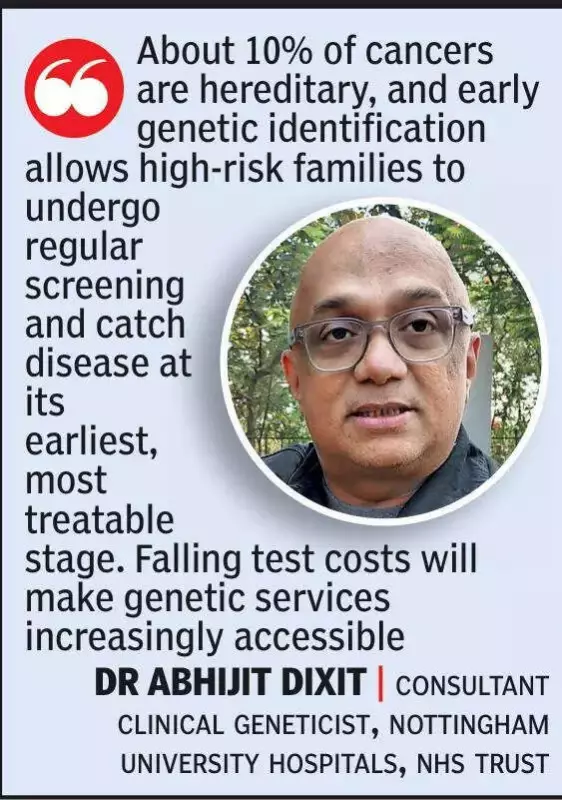
India is on the cusp of a healthcare revolution where genetic science will fundamentally change how diseases are diagnosed, prevented, and treated, according to a leading expert. Dr Abhijit Dixit, a consultant clinical geneticist at Nottingham University Hospitals NHS Trust and honorary clinical associate professor at the University of Nottingham, shared this vision during a recent interaction with clinicians in Nagpur.
The Genetic Medicine Revolution and India's Readiness
Dr Dixit, who contributed to global efforts like the 100,000 Genomes Project, pointed out significant gaps in India's existing genetic infrastructure. Despite these challenges, he emphasized that the field of medical genetics is advancing at an unprecedented rate. Over 200 genetic conditions are now treatable, with new therapies receiving approval every month, dramatically altering the management of rare and complex disorders.
He stated that genetics will soon become a cornerstone of treatment plans across various medical specialties, including epilepsy, oncology, and cardiology. This makes early adoption of these technologies and systemic preparedness critical for India's healthcare future. "About 10% of cancers are hereditary," Dr Dixit noted, explaining that early genetic identification enables high-risk families to benefit from regular screening and early intervention. He added that decreasing costs of genetic tests will make these services more accessible to the population.
Key Challenges: Consanguinity, Delayed Pregnancy, and Data Privacy
Dr Dixit highlighted several pressing concerns for India. He identified consanguineous marriages (marriages between close relatives) as a major medical risk factor. In such unions, the probability of both partners carrying the same faulty recessive gene increases, leading to a 25% chance their child will be affected by a genetic disorder. Overall, this practice raises the risk of genetic disorders by two to four times, which can manifest as hearing or vision loss, developmental delays, or severe multi-organ conditions.
He mentioned that many countries, including some Jewish communities, employ pre-marriage carrier screening to prevent such outcomes. While similar initiatives are emerging in India's sickle-cell-affected regions, widespread adoption is still lacking.
Another trend he discussed is the rising average age of first-time mothers in India, driven by education and career pursuits. With increasing maternal age comes a higher risk of chromosomal abnormalities in offspring. While egg freezing is an available option, Dr Dixit cautioned that it is suitable only for specific situations.
A significant portion of his talk was devoted to the ethical and privacy dilemmas posed by genome sequencing. India currently lacks clear national regulations governing the storage, consent, privacy, and reporting of incidental findings from genetic data. He urged India to develop guidelines similar to those in the US, which specify which actionable conditions must be reported to patients.
Critical Gaps: Newborn Screening and Stem Cell Storage
Dr Dixit expressed concern over the absence of universal newborn screening in India. Many nations routinely test infants for metabolic and endocrine disorders shortly after birth. In contrast, India often misses even basic tests like TSH (Thyroid-Stimulating Hormone), leading to preventable issues such as short stature and developmental delays in children with untreated congenital hypothyroidism.
He also clarified a common misconception, stating that stem cell storage is not necessary for all families and should be considered primarily in high-risk medical cases.
Dr Dixit's insights paint a picture of a transformative yet challenging future for Indian healthcare, where embracing genetic science, bolstering infrastructure, and implementing robust ethical frameworks will be key to improving patient outcomes on a national scale.