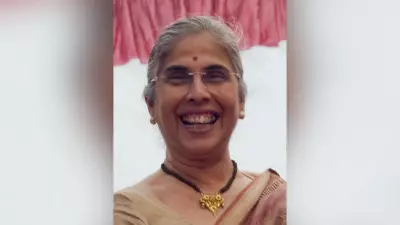
At the age of 40, Medha started suffering from constant abdominal pain and irregular bleeding. She initially dismissed these signs as symptoms of hormonal changes. It was only on her third consultation with a gynecologist that she was advised to undergo a pap smear test. The results delivered a devastating blow: she was diagnosed with Stage III cervical cancer. Despite being educated and having access to information, routine preventive screening had eluded her—it was either inaccessible or, more critically, not a conscious priority.
The Daunting Maze of Treatment and Systemic Shortages
Navigating the healthcare system after her diagnosis proved to be an immense challenge. In India, the stark reality is that there are just two medical oncologists for every one million people, a figure that pales in comparison to the 20-25 per million available in the United States. Finding the right specialist became a confusing journey filled with contradictions. The delay was costly; every 60 days without treatment doubled her medical expenses and significantly increased her risk of death.
Her treatment journey brought with it a heavy logistical and financial burden. Juggling appointments, enduring long commutes, and managing escalating costs became a part of her new reality. Her chemotherapy and radiotherapy sessions take place at a reputed multispecialty hospital. While the quality of clinical care is reassuring, the environment in the general ward is not conducive to recovery. Constant noise, activity, and a lack of privacy make rest nearly impossible. The ordeal is compounded by a grueling 60-minute journey back home in the afternoon heat after each chemotherapy session, which severely worsens her nausea and fatigue.
This arduous experience underscores a critical failure in the system. When detected at Stage I, cervical cancer has a survival rate of 90%. While the age-adjusted cancer death rate has fallen by 33% over the last two decades, cancer is still widely perceived as a death sentence in India, primarily due to late detection. Annually, 2 million patients are diagnosed with cancer in India, yet only 30% of cases are detected in the timely Stages I or II.
Learning from Other Medical Revolutions: Cardiology and Dialysis
The current state of oncology in India mirrors where cardiology was decades ago. Years back, about 2.5 million Indians needed heart surgery each year, but only 12% could access or afford it. The gap was bridged by entrepreneurial cardiac surgeon Dr. Devi Shetty with the creation of Narayana Hrudayalaya. By enhancing cardiologist productivity, optimizing operating room use, and leveraging economies of scale, the hospital chain slashed surgery costs by more than 80% (inflation-adjusted).
Dr. Shetty, who termed this "The Walmart Approach," believes, "Oncology in India is today where cardiology was decades ago. Access is limited, care is expensive, and the need is growing rapidly." He asserts that applying similar rigor, scale, and innovation can transform cancer care delivery.
A parallel can be drawn with the dialysis sector two decades ago. Out of 150,000 Indians diagnosed annually with Chronic Kidney Disease, only 6,000 underwent dialysis due to high costs and limited access. Between 2009 and 2011, companies like NephroPlus and others launched standalone dialysis centers using a capital-efficient model. They expanded rapidly across cities, cutting patient travel time and reducing care costs by 30-40%.
Reimagining Delivery: Decentralized Care and Technology
Today, access to comprehensive cancer care is a major hurdle. Since 60% of patients require a combination of surgery, medical oncology, and radiation, Comprehensive Cancer Centers (CCCs) are the standard. However, these are capital-intensive, with setup costs exceeding INR 500 million, limiting their proliferation. About 60% of facilities are within multispecialty hospitals, where oncology services compete for resources, leading to overcrowding and long waits.
The solution may lie in a distributed network of smaller, asset-light centers offering one or two treatment modalities, bringing care closer to patients' homes. The success of the US Oncology Network, with 600 locations ensuring 40% of the US population has a provider within a 25-km radius, offers a blueprint. Their edge comes from technology: a specialized oncology EHR (iKnowMed) with clinical decision support, patient portals for symptom tracking, and standardized data models that enable value-based care.
In India, pioneers like Dr. Sanket Mehta of Specialty Surgical Oncology (SSO) are building dedicated cancer surgery centers in Mumbai. "Having cancer-specific surgical facilities is critical," says Dr. Mehta. It allows for highly specialized teams, reduces infection risks, and enables investment in complex procedures like HIPEC, all while delivering care more efficiently and affordably.
Bridging the Oncologist Gap and Holistic Support
The shortage of specialists is acute. India has approximately 2,000 surgical oncologists but needs 1,000 more. The gap is even wider for medical oncologists, with only 2,000 available against a requirement of 5,000. While training more doctors is essential, technology can supercharge existing clinicians' productivity. Integrated Electronic Health Records (EHRs) coupled with AI-driven Clinical Decision Support Systems can help generate personalized treatment plans aligned with global protocols.
However, treating cancer is not just about protocols. Dr. Sunny Garg, Chief Medical Officer at Everhope, emphasizes the need for holistic support. "As oncologists, we always strive to treat the whole person, not just the cancer. However, the reality is that we’re often strapped for time," he says. The answer lies in partnering with innovators to address gaps using technology, care managers, and patient-centric systems.
Early diagnosis needs a revolution akin to consumer eye care, where easy access made screenings routine. In India, 70% of patients are diagnosed in late stages. Improving awareness, accessibility, and utilizing tools like AI-powered imaging and multi-cancer blood tests is crucial.
Furthermore, holistic support—like scalp cooling to reduce hair loss, mental health counseling during chemo, and palliative care—is largely missing. Shockingly, 98% of Stage IV cancer patients in India do not receive palliative care to ease their suffering.
Designing for Dignity and The Dawn of New Models
The physical environment of treatment matters profoundly. In many multispecialty hospitals, chemotherapy is administered in shared, noisy wards with little privacy or comfort, as hospitals see lower financial returns from investing in dedicated oncology spaces. Contrast this with world-leading centers like Cleveland Clinic's Taussig Cancer Institute, which uses human-centered design with infusion rooms featuring natural light, art therapy, and quiet spaces.
India needs similar thoughtfully designed centers where chemotherapy rooms are private and services are integrated to reduce patient anxiety. This shift has precedent in maternity care, where chains like Cloudnine transformed delivery into a patient-friendly, premium experience.
Building on these principles, Everhope Oncology was launched in 2025 as a joint venture between W Health Ventures and Narayana Health. It aims to create a network of patient-centric cancer facilities offering surgical and medical oncology closer to patients' homes.
Dr. Pankaj Jethwani, Managing Partner at W Health, notes, "The most forward-looking specialists today are not just exceptional clinicians - they’re entrepreneurs at heart. They deeply understand the patient journey... and are eager to break free from rigid hospital systems to build care models that are not only clinically superior but also more humane and accessible."
The journey of patients like Medha highlights an urgent need for systemic change. By decentralizing care, leveraging technology, maximizing specialist productivity, and designing treatment around patient dignity, India can transform its cancer care landscape and save countless lives through timely and compassionate intervention.