In a significant development for ophthalmology, a new collaborative study has established that a key treatment to halt the progression of keratoconus remains safe and effective even for patients considered high-risk due to associated eye allergies and stem cell damage. The research offers new hope for individuals with this progressive eye condition.
Breakthrough Findings for Complex Eye Conditions
The study, published in the journal Clinical Ophthalmology, was conducted by doctors from Hyderabad's LV Prasad Eye Institute (LVPEI) in collaboration with specialists from the Australian Royal Victorian Eye and Ear Hospital and the Vision Eye Institute. It focused on patients suffering from both keratoconus (KC) and limbal stem cell deficiency (LSCD).
Keratoconus is a disorder where the cornea, the clear front surface of the eye, thins and gradually bulges outward into a cone shape, leading to blurred and distorted vision. The research specifically addressed cases where KC was compounded by vernal keratoconjunctivitis (VKC), a severe, chronic allergic eye disease common in warm climates.
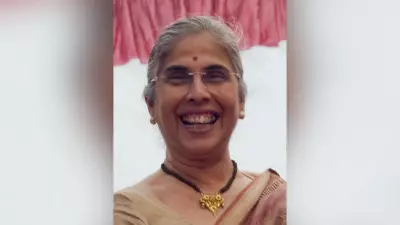
"Frequent and intense eye-rubbing due to the relentless itching of VKC is a major risk factor," explained Dr. Rashmi Deshmukh, lead author and consultant ophthalmologist. "This mechanical trauma can weaken the corneal structure, accelerating keratoconus, and also damage the precious limbal stem cells essential for repairing and maintaining the corneal surface. The resulting deficiency leads to poor healing and scarring."
Examining the CXL Treatment in High-Risk Patients
Collagen crosslinking (CXL) is the globally accepted standard treatment to strengthen the cornea and stop the progression of keratoconus. However, its application in patients with concurrent LSCD had been approached with caution due to concerns about healing.
The research team reviewed the outcomes of 15 eyes from 11 patients who had both conditions. The majority, 14 eyes with partial LSCD, underwent the conventional "epithelium-off" CXL procedure, where the thin outer layer of the cornea is removed. One eye with total LSCD was treated using the "epithelium-on" technique, leaving the surface layer intact.
Positive Outcomes and Clinical Reassurance
The results, monitored over a one-year follow-up period, were highly encouraging. Most patients demonstrated improved vision and a more stable corneal shape. The study recorded a reduction in key corneal curvature measurements, indicating the cornea became less steep and more regular. Notably, the average visual acuity of the patients showed improvement.
A critical finding was that no patient required an additional limbal stem cell transplantation following the CXL procedure, underscoring the treatment's safety profile in this complex scenario.
"Our findings provide strong reassurance," said Dr. Deshmukh. "Collagen crosslinking can be considered a viable option for patients with keratoconus who also have partial limbal stem cell deficiency, provided they are closely monitored post-operatively for any healing-related issues."
This research effectively expands the treatment horizon for a subgroup of patients who were previously managed with extra caution, offering a proven pathway to stabilize their vision and prevent further deterioration of keratoconus.